CIRCULATING VACCINE-DERIVED POLIOVIRUSES (cVDPVs) POLIO AND POOR POST VACCINATION WASTE DISPOSAL
(16 September 2006)
(16 September 2006)
INTRODUCTION
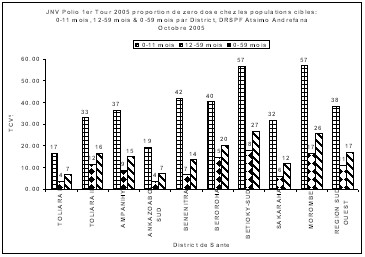
The Active Surveillance system for acute flaccid paralysis (AFP) in Madagascar detected cases of paralytic poliomyelitis due to cVDPVs in Toliara Province in south-western Madagascar from 2001 to 2005. (Rapport du Comité National de certification de l’éradication de la poliomyélite Années 2004 et 2005). In 2005 out of six cases of PFA due to cVDPVs in this Province four were from the Region of Atsimo Andrefana in the Health Districts of Toliara I (1 case), Toliara II (2 cases), Sakaraha (1 case).
The review of literature reveals that
- OPV is genetically unstable; small number of attenuating mutations (vaccine virus still very similar to wild virus) occurs. The mechanism of cVDPVs is believed to be a mutation, or reversion, of the vaccine virus to a more neurotropic form. These mutated viruses are called revertants. Reversion is believed to occur in almost all vaccine recipients.
- Excreted vaccine-derived viruses often are more virulent than the original OPV strains
- Risk factors for emergence of cVDPVs are low levels of population immunity against polioviruses.
- Public health investigations suggest that low vaccination coverage for OPV is allowing cVDPVs to circulate and revert to wild-type characteristics.
- Mass vaccination campaigns with OPV and high routine vaccination coverage for OPV appear to interrupt the circulation of VDPVs
- Contributing factors for cases of AFP due to cVDPVs are low vaccine coverage for OPV in the affected communities, and inadequate vaccination of the affected individuals with OPV.
GOAL
Present the hypothesis that poor post vaccination waste disposal may be a contributing factor for emergence of circulating vaccine-derived polioviruses (cVDPVs).
SPECIFIC OBJECTIVES
- Describe the geographical and physical features of the Health Districts of Toliara I and Toliara II in the Region of Atsimo Andrefana; Fianarantsoa I and Fianarantsoa II in the Region of Haute Matsiatra; and Mahajanga I and Mahajanga II in the Region of Boeny.
- Present the results of injection security investigation.
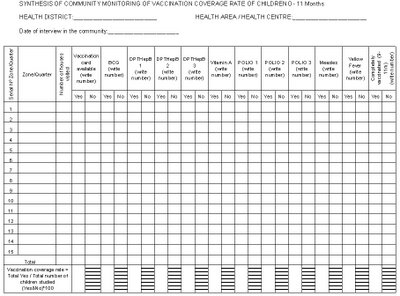
During the STOP Team mission in Madagascar from 24 May to 12 August 2006 the author designed and applied a supervision checklist to assess the process indicators in the implementation of the Expanded Programme on Immunisation (EPI) by health care providers. The components of the supervision checklist were: the cold chain, injection security, monitoring of vaccination coverage rate, supervision and feedback, active disease surveillance, social mobilisation, and community participation.
Only injection security will be considered in this report. The following tasks were investigated at the level of health facilities: recapping of needles, the use of safety boxes, and the disposal of syringes, needles and empty vaccine vials.
RESULTS
a) GEOGRAPHICAL AND PHYSICAL FEATURES OF REGIONS:
- Atsimo Andrefana
It is situated at the south west of Madagascar and is made of nine Health Districts. Toliara I Health District is the urban section of the city of Toliara, the Capital of Toliara Province and Region of Atsimo Andrefana. Toliara is a seaport. Toliara I Health District is in the flat low coastland. Toliara II Health District is the rural part of Toliara city and beyond. It consists of the flat low coastland and hills. Most the rivers in this narrow coastal plain are seasonal. Sakaraha Health District is hilly with fast flowing streams. The Province of Toliara is considered the most arid part of Madagascar. The low coastland is very sandy, flat and submerged underwater during the rainy season from September to March. Pits for waste disposal at Health Facilities in the low coastland are filled by sand during the rainy season and even in the dry season under the influence of wind. - Haute Matsiatra
It is situated in the central high plateau and mountains with permanent rivers; large valleys used for farming especially rice fields. The rivers are fast flowing. The health facilities and residential areas are situated on hills or slopes with very good drainage in all the five health Districts. The soil is solid and hard; pits for waste disposal remain intact until they are full. It has five Health Districts. - Boeny
It has a narrow coastland with undulated hills on the Northern part of Madagascar. Mahajanga is situated on a hill with a narrow coastland. Mahajanga I is the urban section of the city while Mahajanga II is the rural area and beyond. The soil in Mahajanga is hard. The Region of Boeny has six Health Districts
b) INJECTION SECURITY INVESTIGATION
- Toliara I and Toliara II Health Districts, Atsimo Andrefana Region
(14 vaccination health centres supervised)
- Needles are not recapped: 85.7%.
- Syringes and needles are put in safety boxes after use: 92.9%.
- Syringes, needles, empty vials are incinerated: 0.0%.
- Syringes, needles, empty vials are bunt in a pit: 14.3%.
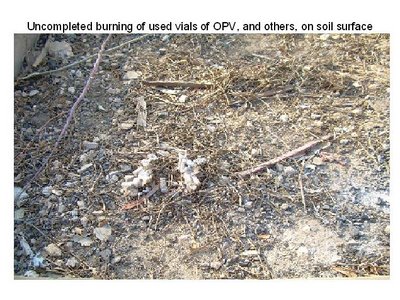
- Syringes, needles, empty vials are bunt on surface of soil: 85.7%.
- Syringes, needles, empty vials are bunt or incinerated immediately after discarding them: 21.4%.
- Safety boxes are bunt or incinerated with contents: 28.6%.
- Fianarantsoa I and Fianarantsoa II Health Districts, Haute Matsiatra Region.
(7 vaccination health centres supervised)
- Needles are not recapped: 100.0%.
- Syringes and needles are put in safety boxes after use: 100.0%.
- Syringes, needles, empty vials are incinerated: 14.3%.
- Syringes, needles, empty vials are bunt in a pit: 71.4%.
- Syringes, needles, empty vials are bunt on surface of soil: 14.3%.
- Syringes, needles, empty vials are bunt or incinerated immediately after discarding them: 85.7%.
- Safety boxes are bunt or incinerated with contents: 85.7%.
- Mahajanga I and Mahajanga II Health Districts, Boeny Region
(3 vaccination health centres supervised)
- Needles are not recapped: 100.0%.
- Syringes and needles are put in safety boxes after use: 100.0%.
- Syringes, needles, empty vials are incinerated: 66.7%.
- Syringes, needles, empty vials are bunt in a pit: 33.3%.
- Syringes, needles, empty vials are bunt on surface of soil: 0.0%.
- Syringes, needles, empty vials are bunt or incinerated immediately after discarding them: 100.0%.
- Safety boxes are bunt or incinerated with contents: 100.0%.
DISCUSSION
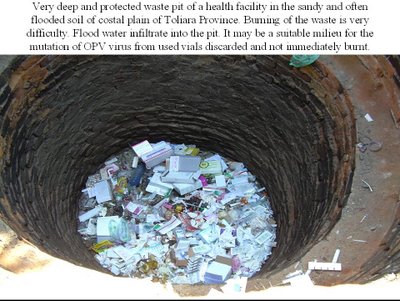
The most important route of transmission of poliovirus from person-to-person is via the faecal-oral route. There is a non negligible environmental element in the transmission cycle of poliovirus. When environmental conditions are suitable cVDPVs may also develop in the environment from discarded vials of OPV that are neither burnt nor incinerated immediately, nor well destroyed. The sandy flooded low coastal plain of Toliara may present an ideal milieu for the development of cVDPVs during the cool rainy seasons. The flooding water which consists of both sea water and fresh rain water from the high lands inland may also be favourable for the environmental mutation of attenuated oral polio vaccine virus. Faecal contamination of the environment during the rainy season is very high in the low coastland because of the flooding. Children and the population in general have the habit of sitting directly and playing on the sand; washing of hands before meals may not often be respected especially amongst children. In the hilly regions waste in the environment is easily swept away by rain water. All the four cases of paralytic poliomyelitis due to cVDPVs in Toliara I, Toliara II and Sakaraha Health Districts have a history of staying in quarters of Toliara before onset of illness.
An excellent elaborate laboratory investigation carried out by the “Institut Pasteur de Madagascar” in Toliara Province confirmed the excretion of cVDPVs in stools of children in quarters/villages of the affected children. No case of vaccine-associated paralytic polio (VAPP) was diagnosed. VAPP is paralytic disease occurring in vaccine recipients, or contacts of recipients of OPV. It is extremely rare.
Cases of VAPP are not linked epidemiologically or virologically to each other but are associated with separate recent exposures to OPV. No case of acute flaccid paralysis due to wild poliovirus was confirmed. It is therefore necessary to sensitize the health personnel and the population on the difference between VAPP and cVDPVs because reticence and refusal to take VPO may be developed.
Cases of paralytic poliomyelitis attributed to cVDPVs have also been detected in Haiti, the Dominican Republic, the Philippines, Egypt, Indonesia and Hong Kong (China); these places may have similar environmental features as the sandy low coastal plain of Toliara; and perhaps the problem of post vaccination waste disposal also.
The results of injection security investigation show that the elimination of post vaccination waste was poorest in the Toliara Health Districts amongst the Health Districts considered, because of the inability of the health facilities to maintain their waste pits that are always filled by sand through out the year. Some of the pits are so deep and protected that burning of the waste is extremely difficult and impossible; water still infiltrate into such pits. Most health facilities in Mahajanga have either incinerators or drum burners, while in Haute Matsiatra the use of pit is prominent.
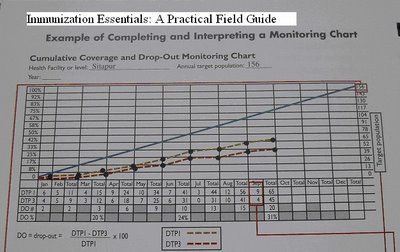
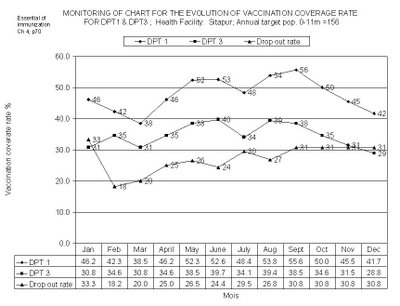
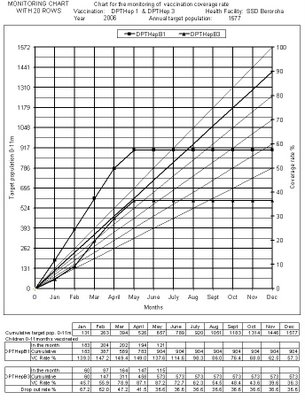
Although the vaccination coverage for the 3rd dose of DPT/OPV at the end of 2005 was high for the three Regions considered, it was relatively low during the first six months of the year.
The results of the vaccination campaign against Polio carried out in October as a riposte to the diagnosis of cases of paralytic polio due to cVDPVs in the Region of Atsimo Andrefana showed a high proportion of the zero doses amongst the 0-11 months 38% for the Region.
The most striking differences between the Health Districts considered of the three Regions were:
- The geographical and physical features – low and often flooded costal plain of Toliara I and Toliara II
- Nature of the soil – sandy soil in Toliara I and Toliara II
Post vaccination waste disposal – poor post vaccination waste disposal in Toliara I and II because pits are easily filled by sand - Environmental sanitation – faecal contamination of the sandy soil during the flooding season, sitting and playing on the soil and non-washing of hands before meals by children
These findings underscore the need for the strengthening of injection security with emphasis in waste elimination in the health facilities situated in the costal plain of Toliara Health Districts by using adapted incinerators.
There is an ongoing effort by the State to maintain high vaccination coverage rate for Oral Polio Vaccine (OPV) amongst children; but this effort may be undermined by the recurrent diagnosis of cases of paralytic poliomyelitis due to cVDPVs that may also be attributed to poor post vaccination waste disposal in this sandy costal plain of the Province of Toliara.
CONCLUSION
“Low routine vaccination coverage is one of the most important causes of VDPV. Because the location of the originating events is unknown, the contribution of other factors is difficult to access; however, a combination two concurrent events within the virus is necessary for cVDPVs emergence; reversion of attenuating mutations to increase neurovirulence, and a presumed increase in transmission characteristics that might be related to recombination with a nonpolio enterovirus. The molecular basis for the second property is not understood”.
In view of the fact that many events concerning cVDPVs are not yet understood, the best approach to reduce or stop the appearance of cVDPVs will be to eliminate all possible contributing factors by ensuring that the defined simplest activities and tasks in the implementation of EPI are correctly performed.
The hypothesis is that the conditions in the sandy and regularly flooded costal plain may be suitable for the environmental mutation of Oral Polio Vaccine virus into cVDPVs. The fact is that post vaccination waste disposal in the sandy and often flooded coastal plain of Toliara Province is poor and difficult to carry out. It would not be exaggerated to say that vaccines and adapted incinerators should be distributed together to health facilities in this Province at high risk; there may be a possibility for all attenuated live vaccines to undergo mutation in such conditions.
The improvement of post vaccination waste disposal should be based on a multisectoral, community, national and international approach, support, participation and commitment in order to eliminate one of the probable contributing factors for the appearance of cVDPVs – poor post vaccination waste disposal. All personnel of health facilities should be trained on injection security especially waste disposal. Good environmental sanitation is primordial.
This report is based on the observation of the author; a more detailed scientific investigation could be carried out; both laboratory investigation indicators and Expanded Programme on Immunization (EPI) process indicators should be assessed in this sandy often flooded coastal plain in Toliara Province and elsewhere also.
This is the author’s modest contribution towards the global eradication of poliomyelitis.
***Related images are found on the next post of the site.***
REFERENCE:
1) Circulation of a Type 2 Vaccine-Derived Poliovirus—Egypt, 1982–1993 Vol 50, No03;41 01/26/2001
2) Pink book 08 Polio CDC.
3) Rakoto Andrianarivelo Mala, Unité de Virologie, Institut Pasteur de Madagascar, Réunion Sahamadio Ilfay Octobre 2005 ; Surveillance des PFA à Madagascar (Janvier – 21 Octobre 2005).
4) Dr Julienne Raneboarisoa – DRSPF à Toliara, PF Surveillance, Rapport de Surveillance Active de la Région d’Atsimo Andrefana
5) Circulation of a Type 2 Vaccine-Derived Poliovirus—Egypt, MMWR 1982–1993 Vol 50, No. 03;41 01/26/2001
6) Public Health Dispatch: Acute Flaccid Paralysis Associated with Circulating Vaccine-Derived Poliovirus—Philippines, MMWR 2001
7) Progress Toward Global Eradication of Poliomyelitis, MMWR 2001 Vol 51, No 12;253 -256, 03/29/2002
8) Public Health Dispatch: Poliomyelitis — Madagascar, MMWR 2002 Vol 51, No 28;622,07/19/2002
9) Progress Toward Global Eradication of Poliomyelitis, MMWR 2002 Vol 52, No 16;366 04/25/2003
10) What STOPers should know about Vaccine-Associated Paralytic Polio (VAPP) and Vaccine-Derived Polioviruses (VDPV) STOP 22 Training CDC, Atlanta May 2006
11) 42 MMWR January 26, 2001
12) World Health Assembly. Global eradication of poliomyelitis by the year 2000. Geneva, Switzerland: World Health Organization, 1988 (Resolution no. 41.28).
13) CDC. Progress toward global poliomyelitis eradication, 1999. MMWR 2000;49:349–54.
14) CDC. Progress toward the global interruption of wild poliovirus type 2 transmission, 1999. MMWR 1999;48:736–8.
15) Vol. 52 / No. 38 MMWR 915
16) Rapport du Comité National de Certification de l’Eradication de la Poliomyélite de Madagascar, Année 2004, Service de vaccination, Ministère de la Santé
17) Rapport du Comité National de Certification de l’Eradication de la Poliomyélite de Madagascar, Année 2005, Service de vaccination, Ministère de la Santé.
***Related images are found on the next post of the site.***